The Joint Annual Scientific Meetings of the Endocrine Society of Australia and the Society for Reproductive Biology 2018
Not your usual case of Low Testosterone (#246)
Mr WM aged 48 years was seen in the Cairns endocrine clinic for evaluation of his hypogonadotrophic hypogonadism. WM’s medical history included new onset hypertension. WM didn’t smoke, avoided alcohol excess and was not depressed. WM reported “muscular fatigue” for 12 months with marked wasting of his quadriceps. WM had very low libido and erectile dysfunction.
WM's mother died at age 52 years from metastatic colorectal cancer. MW had regular surveillance colonoscopies which were normal. His father has essential hypertension.
Clinical examination revealed a BP of 179/111mmHg with a BMI of 24.9kg/m2. He had a round plethoric face with skin thinning, central adiposity and wasting of his limbs. There was also prominent supraclavicular fat pads as well as proximal myopathy. Visual field to confrontation was normal. WM had normal testicles of 25mls.
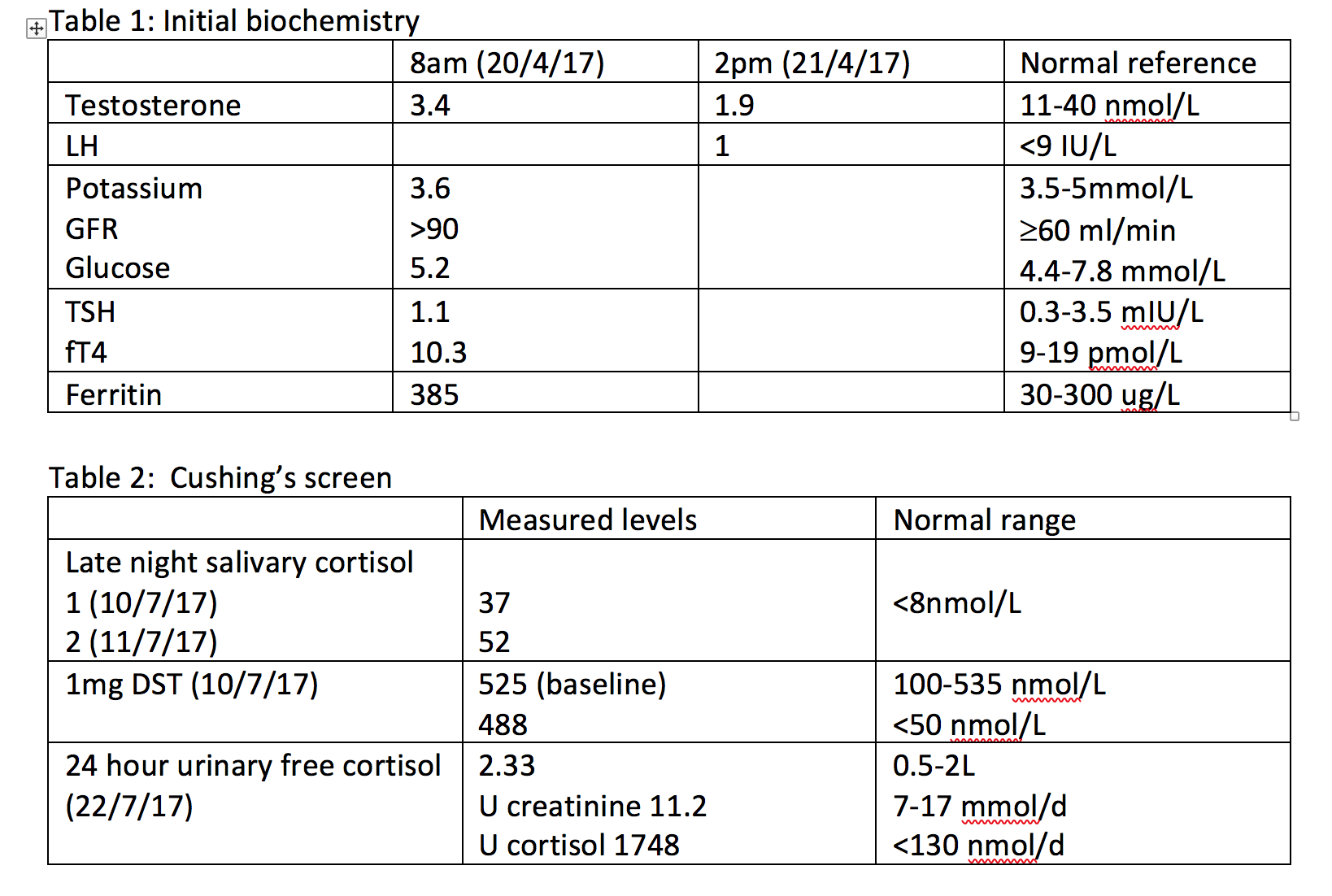
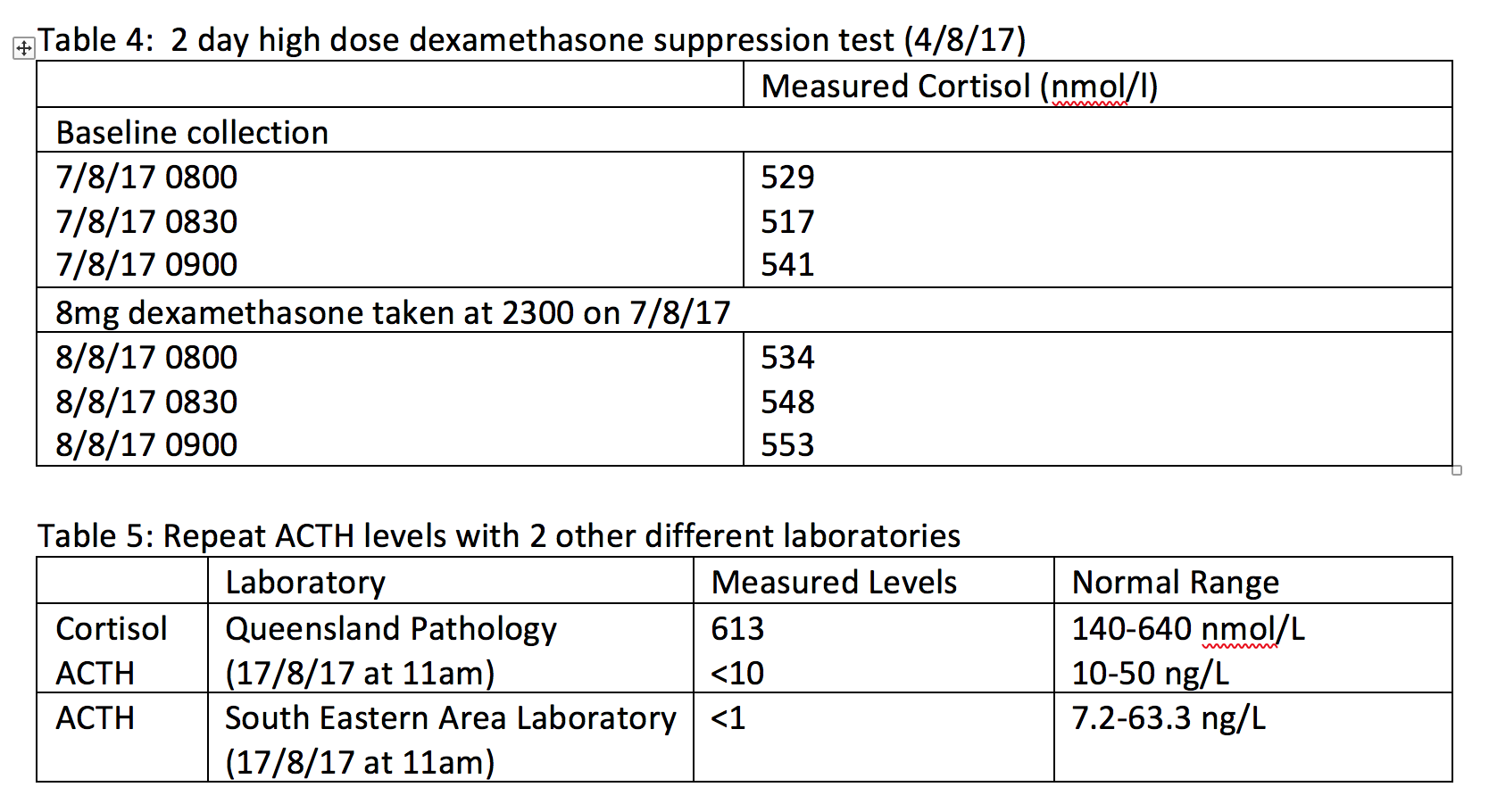
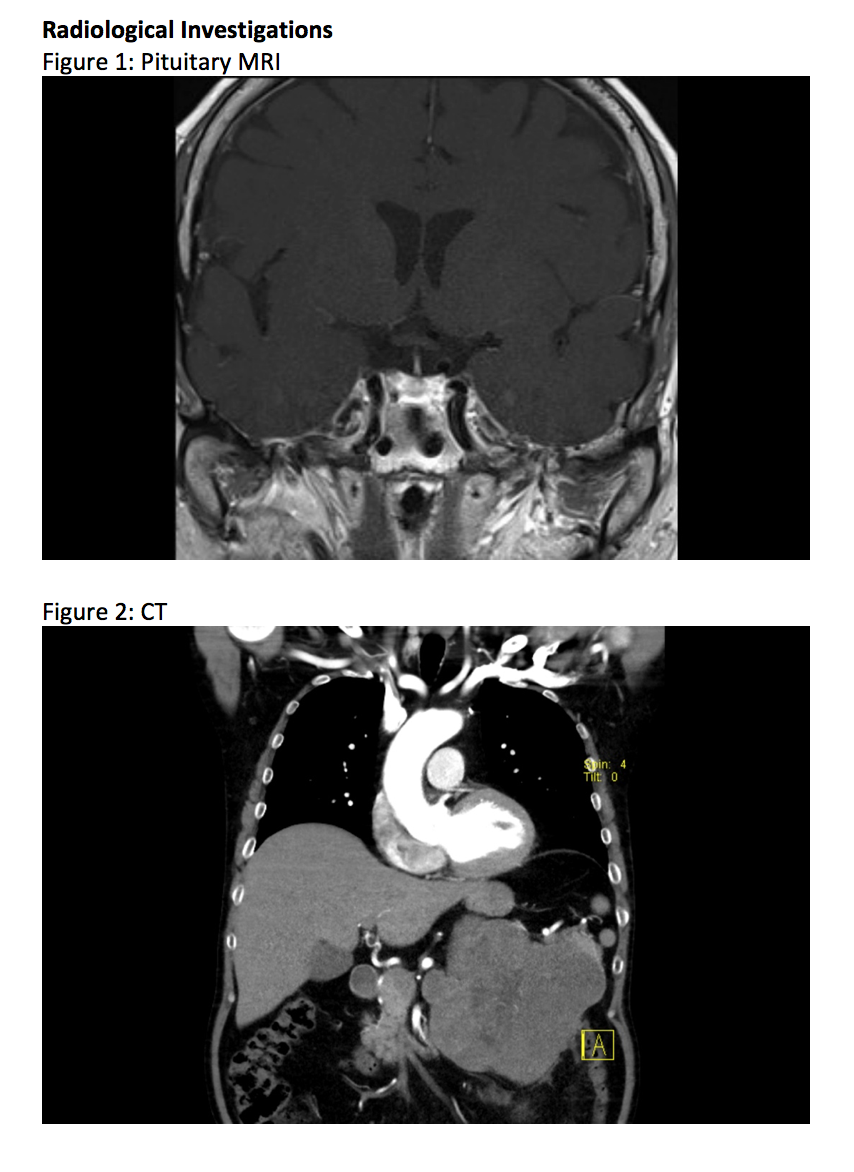
At this point, the working diagnosis was highly suggestive of Cushing’s Syndrome and WM’s Cushing’s Screen showed very elevated late nigh salivary cortisol, no suppression with the 1mg dexamethasone suppression test and a 24 hour urinary cortisol over 13 times above normal. A full pituitary profile showed a measurable ACTH of 11 ng/L and in the presence of WM’s marked Cushingoidism, it was thought the cause was due to ACTH dependence. WM’s pituitary MRI however, did not show an adenoma.
Within a month, WM had rapid escalation of new complications including diabetes, hypokalaemia, fractures, community acquired pneumonia and spontaneous bruising. The working diagnosis now shifted towards ectopic Cushing’s Syndrome with a two day high dose dexamethasone showing a lack of suppression suggestive of this new working diagnosis. Whilst waiting for CRH to become available, a whole body CT was ordered which showed alarmingly a 16.5cm left supra-renal mass in keeping with an adrenal cortical carcinoma which would explain entirely WM’s presentation of hypogonadotrophic hypogonadism and Cushing’s Syndrome.
- Nieman L, Biller B, Findling J et al. The diagnosis of Cushing’s syndrome: An Endocrine Society Practice Guideline. Journal Clinical Endocrinology and Metabolism 2008; 1526- 1540
- Giraldi F, Saccani A, Cavagnini F et al. Assessment of ACTH assay variability: a multicentre study. European Society of Endocrinology 2011; 164 505-512
- Spratt D, Cox P, Orav J et al. Reproductive Axis Suppression in Acute Illness is Related to Disease Severity. Journal Clinical Endocrinology and Metabolism 1993; 1548-1554