The Joint Annual Scientific Meetings of the Endocrine Society of Australia and the Society for Reproductive Biology 2018
Bone microarchitecture in transgender individuals on established cross-sex hormone therapy: A controlled cross-sectional study. (#40)
Background: While sex steroids have complex effects on bone structure, experimental studies suggest that testosterone predominantly regulates trabecular, and estradiol, cortical bone1. The impact of cross-sex hormone therapy on bone in transgender individuals is based on insensitive technology and consequently, existing studies report conflicting effects2. A better understanding of bone effects is paramount given hormone therapy is typically started at a young age and continued lifelong. We hypothesized that estradiol therapy will increase cortical volumetric bone mineral density (vBMD) in male-to-female transgender individuals relative to male controls, while testosterone therapy will increase trabecular vBMD in female-to-male transgender individuals relative to female controls.
Aims: To assess cortical and trabecular vBMD in transgender individuals receiving cross-sex hormone therapy compared with controls.
Methods: High-resolution peripheral quantitative computed tomography (XtremeCT; Scanco Medical, Switzerland) of the radius and tibia was performed in a cross-sectional study of 39 male-to-female and 45 female-to-male transgender individuals on established hormone therapy (at least 12 months). Unpaired students t-test was used to compare transgender individuals with healthy age and birth-assigned sex matched controls.
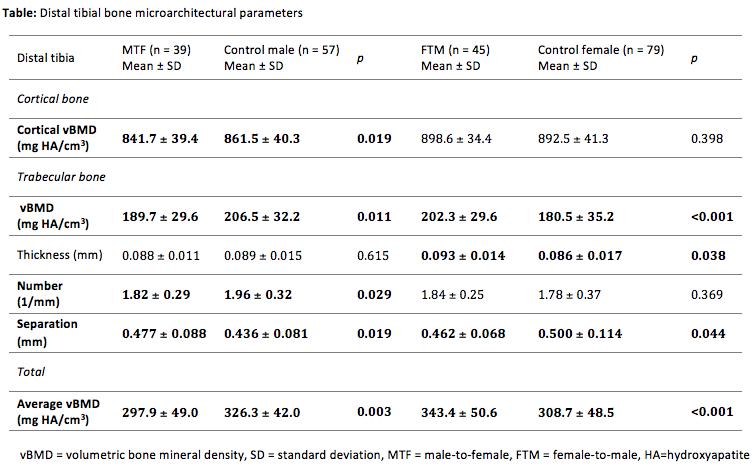
Results: Distal tibial trabecular vBMD (p=0.011) was decreased in male-to-females compared to control males and cortical vBMD was also decreased (Table). Conversely, compared to female controls, female-to-male transgender individuals receiving testosterone therapy had increased distal tibial trabecular vBMD (p<0.001), with increased trabecular number (p<0.001) and decreased trabecular separation (p=0.008) but no significant difference in cortical vBMD. Similar findings were seen at the radius.
Conclusion: The findings in female-to-male (increased trabecular vBMD) and male-to-female individuals (decreased vBMD) support a role for testosterone in building trabecular bone. However, in contrast to our hypothesis, this study of transgender individuals did not confirm a role for estradiol in building cortical bone. Further well-designed prospective studies using sensitive methodology are required to assess long-term bone microarchitecture and fracture risk in transgender individuals.
- Finkelstein, J.S., et al., Gonadal steroid-dependent effects on bone turnover and bone mineral density in men. J Clin Invest, 2016. 126(3): p. 1114-25.
- Singh-Ospina, N., et al., Effect of Sex Steroids on the Bone Health of Transgender Individuals: A Systematic Review and Meta-Analysis. J Clin Endocrinol Metab, 2017. 102(11): p. 3904-3913.