The Joint Annual Scientific Meetings of the Endocrine Society of Australia and the Society for Reproductive Biology 2018
Clinically significant inter-assay discordance in serum prolactin in Australia (#172)
The magnitude of prolactin elevation guides the differential diagnosis of hyperprolactinaemia and parallels prolactinoma diameter. Severe hyperprolactinaemia (>10-fold ULN) is generally due to macroprolactinoma or pregnancy.1 Causes of mild hyperprolactinaemia (<4-fold ULN) include microprolactinomas, dopamine interference, primary hypothyroidism, polycystic ovary syndrome, prolactin co-secretion in acromegaly or Cushing’s disease, and physiological changes (e.g. stress).2-5
We observed eight patients with 28-166% higher prolactin by the Roche versus Siemens platform during routine clinical practice. Some patients had cause for true hyperprolactinaemia but there were no clinical changes in any case to explain the higher Roche levels. For example, a woman with schizophrenia had hyperprolactinaemia at 7-fold ULN by Roche, prompting investigation for prolactinoma. Pituitary MRI was normal and repeat prolactin by Siemens was only 2.5-fold ULN, consistent with her longstanding antipsychotic use.
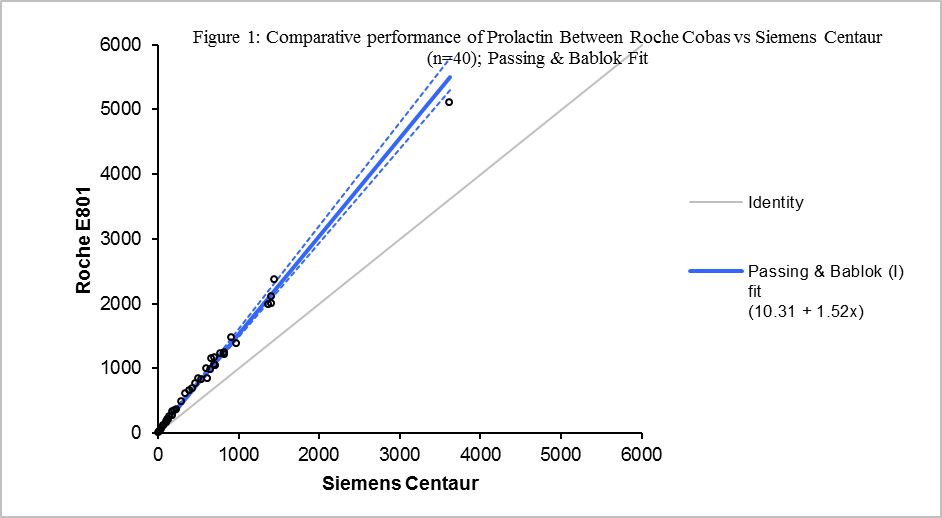
Hence, we measured serum prolactin in both assays using split clinical samples (n=40) across a range of serum prolactin (5-5051 mIU/L). This revealed that serum prolactin was approximately 50% higher by Roche compared to Siemens (Fig 1), despite similar reference ranges. Review of the original Roche data showed no technical error in reference interval calculation; the reason for discordance thus remains unexplained. We speculate that the recent divergence in measurements may relate to either progressive positive bias with successive reagent lot numbers, or antibody deterioration.
Our findings of prolactin inter-assay discordance emphasise the importance of verifying reference intervals and performing bias checks over time. Endocrinologists should be aware of the potential for prolactin overestimation and the utility of repeat testing on different platforms. In mild hyperprolactinaemia by the Roche platform with normoprolactinaemia by other platforms, patients may be spared from unnecessary endocrine reviews and MRI studies. In true hyperprolactinaemia, separating patients with mild versus severe hyperprolactinaemia will narrow the diagnostic possibilities.
- De Sousa SMC, Meyer EJ, Rankin W, Brautigan PJ, Burt MG, Torpy DJ. Vasculogenic hyperprolactinemia: severe prolactin excess in association with internal carotid artery aneurysms. Pituitary. 2017; 20:676-682.
- Vilar L, Fleseriu M, Bronstein MD. Challenges and pitfalls in the diagnosis of hyperprolactinemia. Arq Bras Endocrinol Metabol. 2014; 58:9-22.
- Casanueva FF, Molitch ME, Schlechte JA, et al. Guidelines of the Pituitary Society for the diagnosis and management of prolactinomas. Clin Endocrinol (Oxf). 2006; 65:265-273.
- Melmed S, Casanueva FF, Hoffman AR, et al. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011; 96:273-288.
- De Sousa SMC, McCormack AI, McGrath S, Torpy DJ. Prolactin correction for adequacy of petrosal sinus cannulation may diminish diagnostic accuracy in Cushing's disease. Clin Endocrinol (Oxf). 2017; 87:515-522.